Employers: From ‘Passive Player’ to ‘Change Agent’ in Health Care

Employers are the pivotal players in today’s health care system, yet their role has remained remarkably passive. They can drive meaningful change in the health care market by using their collective influence and speaking with a unified voice. And they need to do so as expeditiously as possible.
Green MPs/Flickr
Amidst so much sound and fury about how to best manage health care in the United States, it’s easy to overlook the fact that nearly two-thirds of all insured coverage is provided by employers, who collectively spend nearly $1 trillion annually on health benefits for their workforces.
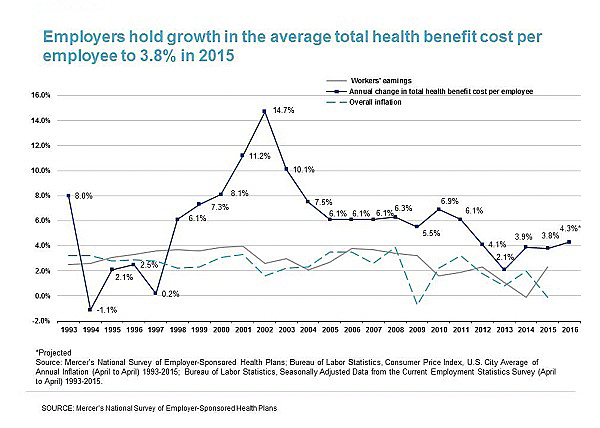
Employers are the pivotal players in today’s health care system, yet their role has remained remarkably passive. Yes, they absorb much of the cost of coverage, ensuring that they are in compliance with the complicated requirements of the Affordable Care Act and other regulations, while they provide many of the tools their employees need as insurance consumers, but a transformation is long overdue. Benefit cost increases outpace overall inflation, and 14.2 percent of payroll is allocated to health care benefits, according to Mercer’s National Survey of Employer–Sponsored Health Plans. Employers can drive meaningful change in the health care market by using their collective influence and speaking with a unified voice.
And they need to do so as expeditiously as possible.
The health care market is entering an era of rapid and continuous disruption. New tech-based entrants are adding more pressure to health plans, which are also facing consolidation pressures. Already, market fragmentation and shifting expectations are bringing more complexity. Alternative care delivery options are emerging, and diverse workforce preferences ensure that one size cannot fit all members.
Meanwhile, the promises of cost savings from genomics and personalized medicine haven’t yet been realized, and more restrictive plan designs and networks available on the public exchanges are likely to foster greater inequality among health care consumers. A new health market is emerging, and employers must capitalize on this formative period to redefine their role and shape the market to meet their strategic objectives.
Health Care Transformation and the Workforce
The need for health care transformation is underscored by another simple fact: A healthy workforce is strongly aligned with business success in such areas as increased productivity, reduced absenteeism, higher retention and better overall engagement. Historically, companies with superior wellness programs outperform the S&P 500 Index. Still, the current system is too often failing its stakeholders in terms of cost, quality and satisfaction.
An influential report from Health Affairs estimated that 34 percent of U.S. health care spending is wasted. A recent study from Johns Hopkins University suggested that medical errors are the third leading cause of death in the U.S. As for satisfaction with the health care system, the 2016 B2C NPS benchmarking report shows that health plans rank in the bottom quartile of business-to-consumer services.
The evidence of escalating costs, wasteful spending, quality gaps and abysmal satisfaction ratings is driving the need for transformation. Employers cannot rely on other stakeholders to drive change. Consumers, after all, don’t have a unified voice, and government solutions bog down in issues of political will and philosophy. Fortunately, there are steps that employers—of any size—can take to make a difference and transform from passive players to change agents.
Employers can lead the transformation through a collective focus on four vital aspects of positive change:
- Pay for Value. This means aligning reimbursement of medical claims with value, not volume. Employers should pay for better patient outcomes, more efficient care and an improved member experience. It will require them to know what percentage of their workforce is cared for by providers with value-based reimbursements models, such as accountable care organizations and patient-centered medical homes, and how much they are receiving in additional fees. Reporting of value-based reimbursement models must be built into carrier contracts and proposals.
- Drive to Quality. It’s delivering the right care at the right time, in the right setting, error-free. Employers must inventory all sources of quality information from current vendors, know where the workforce is receiving low-quality care, evaluate plan design options to create a meaningful cost differential between seeking care at high- and low-quality settings and modify carrier contracts to exclude payment for “never events” (serious negative outcomes that are preventable).
- Personalize the Experience. This means leveraging better data and technology to engage employees in the right behaviors every day, not just when care is needed. Employers must hold vendors accountable for achieving high customer satisfaction via a performance guarantee, offer services that provide high-touch/high-tech support to help employees become more empowered consumers and create basic expectations of what their workers want and value in health care design, all in recognition that their employees are their customers when it comes to benefit offerings.
- Embrace Disruption. Inject change into the system, even if it creates short-term disruption. Employers must assess and score how each vendor partner aligns with strategic objectives; define expectations for all vendor partners, establishing discipline and agreeing to a cadence for measurement and reporting; review procurement and contractual requirements associated with out-clauses and forming new partnerships if current partners aren’t delivering and make the business case for change with internal leaders, socializing the business imperative.
There’s a long road ahead to meaningful change, but committing to this four-pronged strategy today is the first step. It has the potential to ensure a better tomorrow for all stakeholders.