Health Care Industry Disruption Pressures Insurers To Evolve

A man consults his doctor online as he waits for tourists to have a digital photo taken against Hong Kong's famous skyline. Technology companies in Asia are building digital platforms to rapidly offer integrated health care services.
Photo: Peter Parks/AFP/Getty Images
This is the first article in a special series focused on health-related issues.
In the past, health care incumbents—traditional health insurers, hospital providers, and pharmaceuticals and device manufacturers—negotiated costs and fees in a black box, and consumers had little say. Like many industries, however, health care has been disrupted by the introduction of digital technology, which is enabling the use of advanced analytics for many applications, such as increasing cost, care quality transparency, and greater access and choice, for both clinicians and consumers. Inspired by global trends, Asia, too, has a thriving digital health ecosystem: Many new startups and disruptors have entered this space, with 294 Asian health-tech funding deals closed in 2018 alone.
The balance of power, decision-making and transparency has started to shift from physicians to consumers, creating new sites of care at home and in the cloud. In this new environment, health care incumbents must now defend their relevance and compete with digital players for a share of the growing consumer spend on health. Health insurers are not only paying for sick care in the hospital setting, but they are also increasingly funding unconventional methods of care—virtual, home-based, and even simple machine learning or artificial intelligence, such as AI “doctors” and symptom checkers.
The role of health insurance is being reshaped by three market forces. First, insurers are moving from products to services: from traditionally reimbursed medical expenses and procedures to integrated services, ranging from lifestyle-related benefits to condition management. Second, insurers are opening up new customer segments by offering personalized products and features tailored to different member needs and specific membership bases. Third, the shift from clinical to consumerized will accelerate with the democratization of data through greater access to health records, provider ratings and self-diagnosis tools. Governments may need to play the role of the catalyst, as pricing transparency can help level out costs between public and private facilities.
What Are the Implications for Insurers in Asia?
Amid such market forces, health insurers risk losing market share if they fail to adapt. At the same time, the rapidly changing landscape provides an opportunity for insurers in Asia to break down traditional boundaries and adopt new roles and business models.
The health insurance offering in Asia has not changed dramatically for decades. Basic programs usually cover inpatient services only and exclude preventive services and screenings, outpatient medicines and holistic care. Member coinsurance and copayment are not standard, and health records and many processes—from eligibility to claim submission—are still paper-based. The relatively large gap between health insurance in Asia and mature markets presents significant growth opportunities for insurers to do the following:
Expand the portfolio. Offer completely new health products or features beyond basic indemnity and deliver more value for members.
Broaden the market. Access untapped, previously uninsured members, especially as digital channels and partnerships create new introductory touchpoints.
Differentiate to compete. Offer exclusive services and privileges, which can help gain market share.
Consumer appetite for innovation is also growing. Private health insurance customers in Asia are looking for services, such as wellness benefits, that are differentiated from public (or universal) health care, which is often associated with poor user experiences. Insurers can instead focus on the long game and build loyalty from early on with new members. For example, wellness platforms will present opportunities to foster trust and associate an insurer’s brand with delightful experiences and rewards while members are healthy, rather than being exclusively associated with often unpleasant claims and interactions. Insurers can also collect data on behavior and life event signals, enabling them to approach members at appropriate times for considering new insurance products, such as starting a family.
Some broader environmental characteristics in Asia could enable the region’s insurance industry to leapfrog into the digital health age. Many of the world’s leading health technology companies are now based in Asia, and insurers benefit from this proximity, as has happened in China’s rapidly digitizing health care market. Investment in health technology is growing rapidly: at a compound rate of approximately 50 percent in Asia-Pacific between 2014 and 2018, compared to 18 percent in the U.S. Also, many countries in Asia have regulatory environments that enable digital proliferation: For example, Singapore has introduced a fintech regulatory sandbox to drive innovation, including in the insurance sector.
However, incumbents face competitive pressure from big global and Asian technology players, as well as from other industries. Technology companies are building digital platforms to rapidly offer integrated health care services like telemedicine and smart devices to their large membership bases, and telecom operators have even entered health care by providing privileged access to digital health services. Insurers have assets they can leverage—particularly their scale and large membership bases—to fight off some of these threats and extend their role in the patient journey. However, doing this alone will be challenging, given the significant investment required to develop new capabilities and attract the right talent.
Insurer-Digital Partnerships To Build Health Ecosystems
Conventionally, health insurers only have contact with members at the end of an illness event. Extending earlier into the patient journey before claims are incurred or even before any illness, has the added potential benefit of avoiding or reducing future claims. Health insurers can participate earlier in the patient journey through partnerships with providers of complementary capabilities or by building these themselves. Insurers are also playing a larger role in connecting patients to the right care once they become sick and in ensuring they receive optimal treatment. Finally, insurers can offer recovering patients additional support to manage chronic diseases and take medicines at home.
In these partnerships, insurers provide scale and access to a captive membership base, while the startups provide new capabilities and services beyond the insurer’s core competencies. They can make this new value available to their members without having to shoulder significant investment to build it in-house. Furthermore, combining various partnerships into one integrated user experience forms the beginning of an important business-to-consumer health ecosystem, which provides opportunities for more member touch points and paths to influence or enable better care. Building their own health ecosystem redefines the role of the insurer with the goal to integrate services with core insurance products, leverage data and analytics across services, create a seamless user experience and coordinate care between each step of the journey.
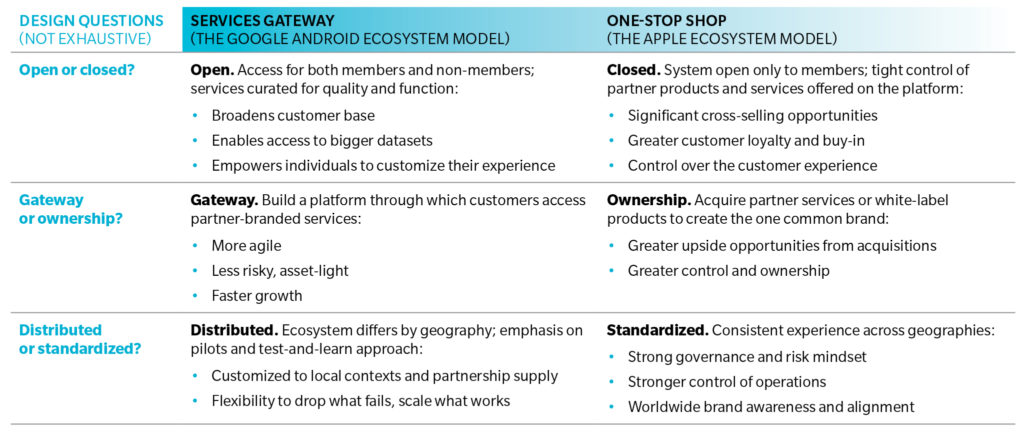
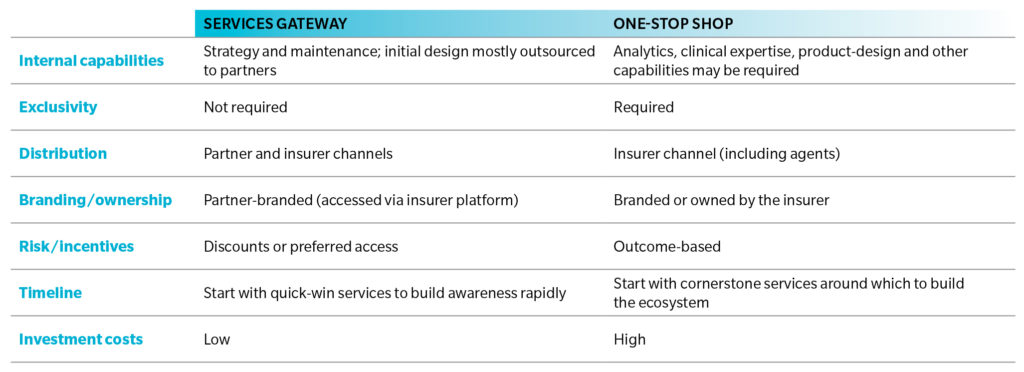
To develop these new consumer-focused health ecosystems, insurers will first need to design their objectives and ambitions in the spectrum of approaches between becoming a services gateway (the Google Android ecosystem model) and a one-stop shop (the Apple ecosystem model). Then insurers will need to select the right partners to offer the component services, either with a large number of companies iterating rapidly in the gateway model, such as ZhongAn, or longer-term exclusive partnerships to develop a one-stop shop, for example, Prudential and Babylon Health. Finally, insurers must consider go-to-market approaches that best fit both the specific partnerships and the overall ecosystem model.
Exhibit 1: Design Questions for Ecosystem Approaches
Exhibit 2: Go-to-Market Considerations
Digitization and consumerization themes have already penetrated the health care industry in Asia, and many new insurer-digital health partnerships have emerged. While partly defensive, these collaborations also present new opportunities for value creation for both consumers and insurers. However, Asia’s insurers will also need to temper their ambitions with an understanding of both risk and investment required in such a strategy.
Read the full report here.